
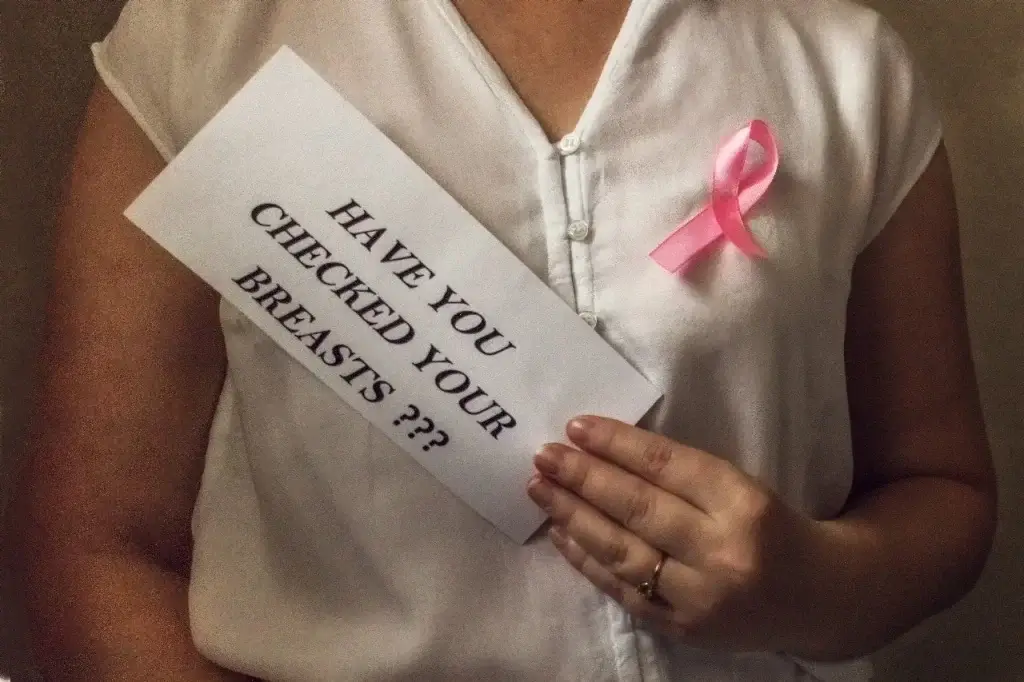
When I first decided to write this, it was for the friend who had just felt a lump and the sister still worried even after a clean scan. It was for us. Because while we’ve all heard the common messages around self-checks and mammograms, the true picture of what may raise our risk of Breast Cancer is much more layered, more human, and yes—sometimes surprising.
Today, let’s walk together through what the research says about the causes (or more accurately, the risk-factors) of breast cancer. We won’t promise certainty—no expert does—but we will shine a light on lesser-talked-about triggers and what we might gently do about them.
First, a truth worth knowing: there is no single cause of breast cancer. As the Centers for Disease Control and Prevention (CDC) explains: “Your risk … is due to a combination of factors.
And the World Health Organization (WHO) adds that around half the women who develop breast cancer don’t have any of the identified risk factors beyond being female and ageing.
So yes—in part we’re wrestling with probabilities, not guarantees. But understanding the triggers helps us lean into what we can influence.
Because we’re writing to you as women, we begin with the elements we can’t change—but can deeply understand.
Family history & gene mutations. Mutations in genes like BRCA1 and BRCA2 are well known to raise breast-cancer risk. Still: inherited gene changes account for only about 5-10% of all breast cancer cases.
These are the “background” factors. But now let’s move into the parts of the story we can act on—and the places where new research is reshaping what we thought we knew.
Here are several factors within our everyday lives—some obvious, some less so—that research shows play a role in breast-cancer risk.
It’s one we often under-estimate. According to the American Cancer Society (ACS), drinking even just one alcoholic drink a day is linked with a 7-10% higher risk of breast cancer compared with none; drinking 2-3 drinks daily raises it more.
Why? Alcohol influences oestrogen levels, damages DNA and may increase breast-cell susceptibility to carcinogens.
This doesn’t mean you can never enjoy a glass. But awareness counts—if you have other risk-factors, reducing alcohol becomes even more important.
Being overweight has a stronger link with breast cancer after menopause. Here’s why: after menopause the ovaries stop producing most oestrogen; fat tissue becomes a bigger source of oestrogen, which can stimulate breast-cell changes.
The bottom line: maintaining a healthy weight isn’t just about appearance—it’s a stronger protective step than many realise.
The body loves being in motion. Regular exercise is emerging not just as good for energy and mood but for breast-cancer risk reduction. The ACS suggests adult women aim for 150-300 minutes of moderate activity weekly.
Why it matters: movement may moderate hormone levels, reduce inflammation, and keep body weight in check—all protective pathways.
Using hormone replacement therapy (HRT) for menopause symptoms that combine oestrogen and progesterone has been associated with higher risk.
Similarly, some studies show a slight risk increase with oral contraceptive (birth-control) pills while using them, though that risk seems to fade over time.
This is not about alarm—it’s about informed conversations with your doctor.
These are the ones we rarely hear about—but as modern research gathers, they’re increasingly important.
We live surrounded by hormone-mimicking or hormone-altering chemicals: in plastics, personal-care products, pesticides. While research is ongoing, mounting evidence suggests these may raise breast-cancer risk via hormone disruption or by making breast tissue more sensitive.
For example: ultra-processed foods, exposure to industrial “forever chemicals”, even light at night (which disrupts circadian rhythm) have been discussed as possible triggers.
What can we do? We can’t live in a bubble—but we can choose fewer plastics in food storage, opt for minimal-fragrance cosmetics, reduce ultra-processed-food intake, and prioritise sleep (more on that soon).
It’s not always as direct as “stress causes cancer” but chronic stress, poor sleep, and night-shift work may disrupt hormonal regulation and immune surveillance. Some studies identify night-shift work (disrupting melatonin production) as a probable carcinogen for breast cancer.
Even though we can’t completely eliminate stress (hello, life!) we can build coping, prioritise restful sleep, and minimise night-time light exposure.
As more women delay childbearing, have fewer children, or breast-feed for shorter durations—as is common in many parts of the world—these shifts can subtly influence breast-cancer risk.
Breast-feeding for a year or more is linked with a modestly lower risk. Pregnancy at younger age and more children (in older demographic data) were protective—but that doesn’t mean you must do “more” than you’re comfortable with. It means knowing this factor, being aware, and working other protective elements.
Alright—so many of us reading this will sigh: “I don’t have all of these risk-factors, and yet…” That’s because risk is just that—a chance, not a certainty. Many women with breast cancer have few or none of the recognized risk factors. The flip side: many women with multiple risk factors never develop it.
Here are some compassionate, realistic steps we can take today, together, as women caring for our bodies and our futures:
Get to know your body: breast-self-checks, know your normal, ask questions. Early detection saves lives.
Talk openly with your doctor: about your family history, your hormone therapy use, your reproductive history.
Choose movement: If you can just start with walking 30 minutes most days—great. Build up.
Moderation with alcohol: If you drink, consider cutting back. It’s one of the modifiable risks.
Sleep + manage stress: Prioritise 7-8 hours of restorative sleep, practice stress-reduction (yoga, meditation, shared talk with friends!).
Smart choices on environment: Minimise exposure to plastics, opt for less processed food, reduce exposure to chemical-heavy personal-care products, improve sleep hygiene (less screen time near bedtime).
Maintain a healthy weight: If you’re post-menopause—or getting there—it becomes extra important.
Breast-feed if you can & choose as full-term a pregnancy pattern as life allows: These are factors but only a part of the picture.
Often when we talk about breast cancer risk we hear: “Check your genes, check your age, check your family history.” Those are absolutely valid. But the “hidden” or “surprising” triggers are the ones we can under-look—environmental chemicals, sleep disruption, lactation patterns, modern reproductive shifts.
When you’re a woman juggling career, family, societal expectations, personal aspirations, and health—it matters more that you see the full landscape. Because prevention isn’t about perfect—it’s about persistent, gentle steps. It’s not about fearing the future—it’s about choosing small daily acts of care.
If you’ve ever wondered whether it’s your fault (it isn’t). If you’re feeling overwhelmed by the list of “what increases risk” (you’re not alone). If you’ve carried worry in your heart for your body, your sisters, your daughters (thank you for reading this)—here’s a message: You are doing enough when you engage, when you choose quietly each day to care for yourself.
And if you face a breast-cancer diagnosis (either personally or for someone you love)—know this: your value is not defined by what your body does or what it faces. Detection early, support relentlessly, treatment boldly: these threads weave hope.
In summary: The causes of breast cancer are many–an interplay of genetics, environment, lifestyle, reproduction, and unknowns. We cannot control everything—but we can influence many factors with compassion, awareness, small steps. And as women for women, we walk this path together.
Take care of your body, cherish your life, lean into community. And above all: let’s keep the heart-to-heart talk going. Because knowledge shared is hope multiplied.
With warmth and sisterhood,
Your fellow woman who cares.
Surprisingly, yes. The gut microbiome influences how our body metabolizes estrogen — one of the key hormones linked to breast cancer. When gut bacteria are imbalanced (a state called dysbiosis), excess estrogen can circulate longer in the body, potentially raising risk. A fiber-rich diet, fermented foods, and limiting processed sugar all help nurture a “protective” microbiome. Think of it as supporting your second brain and your breasts at once.
Yes, growing evidence links disrupted circadian rhythm — the body’s natural sleep–wake cycle — with higher breast cancer risk. The World Health Organization has even classified night-shift work as a “probable carcinogen.” Reduced melatonin from light exposure at night can influence estrogen regulation and DNA repair. Prioritizing dark, consistent sleep helps protect your hormonal rhythm.
Some may be. Certain endocrine-disrupting chemicals (EDCs) — like parabens, phthalates, and BPA — can mimic or interfere with hormones that influence breast tissue. While evidence varies, studies increasingly point toward a connection between long-term exposure and higher risk. Choosing fragrance-free, “paraben- and phthalate-free” products and avoiding plastic microwaving are small but meaningful steps.
Yes — and it’s one of the most surprising modern factors. Artificial light at night (from screens, lamps, and even streetlights) suppresses melatonin, the hormone that helps regulate sleep and may have anti-cancer effects. Studies link night-shift workers and chronic late-night screen users with higher breast-cancer risk. Try to dim lights two hours before bed and sleep in a dark, device-free room — a gift to your circadian rhythm.
Emerging science says possibly yes. Fine particulate matter (PM2.5) and certain traffic-related pollutants have been shown in several studies to raise estrogen levels and oxidative stress — both connected to breast-cell changes. While we can’t move mountains (or cities), using indoor air filters, adding plants like peace lilies, and taking “green breaks” outdoors can make a subtle but meaningful difference.



 ×
×

