Is Hormone Replacement Therapy (HRT) Right for You?
A Comprehensive Guide to Hormone Replacement Therapy
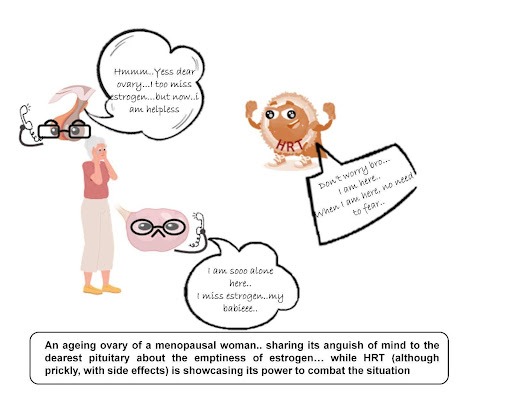
Hormone Replacement Therapy (HRT) is gaining significant attention for its role in managing bothersome symptoms during menopause. This comprehensive exploration of HRT will address its fundamentals through the “5 Ws” (What, Why, Who, When, and Where), along with its benefits and potential side effects.
What is Hormone Replacement Therapy (HRT)?
HRT involves administering hormones that the body no longer produces in adequate amounts, typically during menopause. The fluctuating and declining levels of estrogen and progesterone trigger various troublesome symptoms, such as hot flashes, night sweats, mood swings, sleeplessness, anxiety, vaginal dryness, and painful intercourse. HRT supplements these hormones to alleviate symptoms. Besides menopause, HRT is also prescribed for treating hypogonadism or for those undergoing gender transition.
Why Do Hormones Slump During Menopause?
The primary reason for the hormonal decline is ovarian aging. As women reach their 40s and 50s, the number of ovarian follicles decreases, and the ovaries become less responsive to hormones, leading to reduced production of estrogen and progesterone. This hormonal deficiency triggers menopausal symptoms.
How Does HRT Work?
Based on the patient’s health history, a medical practitioner determines whether a combination of hormones (estrogen and progesterone) or a single hormone is needed. Endogenous estrogen regulates the menstrual cycle, fertility, vaginal health, bone density, skin elasticity, cardiovascular health, and mood. At the same time, progesterone prepares the uterus for pregnancy, balances the menstrual cycle, and supports neuroprotection. HRT mimics these endogenous hormones to counter the physiological effects of menopause.
Types of Hormone Replacement Therapy (HRT)
HRT comes in various forms tailored to individual symptoms and preferences:
1. Estrogen-alone HRT
A woman experiencing menopausal symptoms after a hysterectomy (surgical removal of the uterus) is prescribed estrogen therapy alone, as exogenous progesterone supplementation is not necessary. To restore hormonal balance, the therapy consists of taking only estrogen supplements. It assists in controlling body temperature, which lessens the frequency and intensity of night sweats and hot flashes. Additionally, it aids in keeping the vaginal walls lubricated and elastic while avoiding dryness.
2. Combined HRT
For women who have not had surgery and have an intact uterus, the therapy consists of progesterone and synthetic estrogen supplements taken together. Routine monitoring and consultation with healthcare professionals is a useful method of managing menopausal symptoms and preserving endometrial health.
Further, it can be used in two ways:
- Sequential Combined HRT: A combined regimen for treating the symptoms that involve continuous and cyclical estrogen and progesterone administration is known as sequential or cyclic hormone replacement therapy (HRT). Usually, women with an intact uterus who are in the perimenopause or early stages of menopause are administered it. The idea behind using progesterone cyclically is to help shed the endometrial layer (uterine lining) and cause withdrawal bleeding similar to that experienced during menstruation. This helps prevent hyperplasia and relieve menopausal symptoms.
- Continuous combined HRT: Progesterone and estrogen are taken consistently each day in this kind of combined hormone replacement therapy. It is administered to postmenopausal women to stabilize their hormone levels; however, it also needs to be properly monitored to assess individual risk factors, such as a family history of genetic disorders, the risk of long-term use, and cardiovascular health to prevent blood clots and strokes.
3. Local HRT
During this regimen, hormones—typically estrogen—are applied locally to the vaginal region via pills, creams, gel, patches, and rings. The main objective of these products is to minimize systemic absorption while providing targeted relief for menopause-related symptoms related to vaginal and urinary health. It is usually prescribed to postmenopausal women.
4. Bio-identical HRT (BHRT)
Synthetic and natural hormone replacement therapy (HRT) derived from plants that share structural and functional similarities with the estrogen produced by a woman’s body is known as “bio-identical HRT.” They support the control of physiological processes by acting as an estrogen substitute. BHRT comes in tablet, cream, gel, patch, and pill form.
Why Consider HRT?
HRT is beneficial for managing menopausal symptoms and improving the quality of life for aging women. It is particularly advantageous for working women who need to manage menopause while maintaining their professional responsibilities. Benefits include better concentration, emotional stability, and overall well-being, leading to enhanced productivity and performance.
Who Should Consider HRT and Who Should Not?
While some women find it to be an extremely effective treatment for managing disruptive symptoms and averting long-term health problems, it might not be appropriate for everyone. Given that the best decision for each individual is different, it is crucial to have a prior discussion regarding taking HRT with a healthcare provider.
Suitable Candidates for HRT
- Women under 60 years old or those who have been menopausal for less than 10 years.
- Women who are experiencing severe and frequent hot flashes, night sweats, mood swings, and other symptoms.
- Women who have undergone hysterectomy before age 40 are more susceptible to severe symptoms and osteoporosis.
Unsuitable Candidates for HRT
- Women with a history of breast cancer or familial breast cancer.
- Women with blood clotting disorders (e.g., deep vein thrombosis).
- Women with uncontrolled hypertension.
When to Start HRT
The optimal time to initiate HRT is within a decade of menopause onset or before reaching 60 years of age. Early initiation is more effective in alleviating menopausal symptoms and preventing osteoporosis. Starting HRT later, beyond 60 years, is associated with higher risks, particularly cardiovascular disorders.
Where to Get HRT
Gynecologists and endocrinologists are the primary healthcare providers for HRT. After thorough examinations, HRT can be obtained from clinics, hospitals, or specialized HRT centers.
Risks and benefits of Hormone Replacement Therapy (HRT)
Menopausal symptoms can significantly impact quality of life, but Hormone Replacement Therapy (HRT), considered the gold standard for treatment, can alleviate these issues. However, it is important to recognize that, alongside its benefits, there are adverse effects of hormone replacement therapy.
Benefits:
- Reduces hot flashes, night sweats, sleeplessness, vaginal dryness, and discomfort.
- Maintains bone density, reducing the risk of osteoporosis and fractures.
- It alleviates mood swings, depression, and anxiety.
- May reduce cardiovascular disorders and hypertension (though still debated).
- Improves urinary symptoms like urgency and incontinence.
- Maintains skin elasticity and moisture.
- Enhances overall well-being in middle-aged women.
Risks:
- Mood disturbances, including increased mood swings and irritability.
- Breast tenderness and enlargement.
- Bloating, nausea, and headaches.
- Increased risks of thromboembolism and pulmonary embolism.
- There is a higher risk of breast, ovarian, and uterine cancer with long-term use.
- Elevated risk of cardiovascular disorders and stroke, especially in older women.
Alternatives to HRT
For those who prefer not to undergo HRT, other options include:
1. Lifestyle Modifications:
- Adopting a balanced diet rich in phytoestrogens (found in fruits, vegetables, whole grains, pulses, soy, and linseed) to reduce menopausal symptoms.
- Regular exercise, yoga, breathing techniques, and meditation reduce stress and anxiety, improving overall well-being.
2. Non-Hormonal Treatments:
- Selective Serotonin Reuptake Inhibitors (SSRIs) for managing depression, hypertension, and anxiety associated with menopause.
3. Herbal Remedies:
- Medicinal plants rich in phytoestrogens, such as licorice, red clover, Vidarikand, Asoka, Brahmi, and Manjistha, mimic estrogen and help regulate hormonal balance without side effects.
Final Thought
Hormone Replacement Therapy (HRT) is a valuable treatment for managing menopausal symptoms and improving quality of life. While it offers numerous benefits, it also has potential side effects and risks. Therefore, a thorough discussion with a healthcare provider is crucial to determining the best approach. Alternatives, like lifestyle modifications and herbal remedies, can also provide relief for those who prefer not to use HRT. Making an informed decision based on individual health history, symptom severity, and personal preferences is essential for optimal outcomes.
At Miror, we understand the unique challenges women face during perimenopause and menopause. Revive is designed to support you through this journey, empowering you to live your best life. Visit our website to learn more and take control of your health today!




